Let me start by answering some FAQ’s I’m getting with respect to neurofeedback.
Does it have to be the Othmer’s system? There are quite a few choices of systems on the market. I am out of date, because I am just starting to reconnect with old friends in the neurofeedback community, or should I say communities. The Othmer’s new system, Cygnet, does what the others do, plus it is able work at the “ultra low frequencies” that Sue is using in her clinic. They also have a tight network of practitioners who share clinical experiences on a private listserve and consult with Sue about particular patients if needed. It allows me, for example to start a patient here and have them follow-up with someone close to them at home who has the same equipment and uses the same protocol, though, as I said before, it is not a one size fits all protocol. Unfortunately. Judgement is required. It’s getting closer and closer though. It’s fun to think about a future with wireless electrodes and one size fits all neurofeedback that anyone can do anywhere, on their iPhone.
BrainMaster used to give the most for the least money. A quick look at their website and it looks like they still do. I also had a little experience with Roshi and LENS, but I consider them to be in a different category, because they use stim to entrain the brain. It is a powerful technique, but I don’t have enough experience with it personally to write about it or advise strangers to try it. There are many testimonials out there for those techniques, however. They fall into the category of things that could help so many people, but will never be studied, because it doesn’t fit into the dominant paradigm and there isn’t enough money to be made, unless people start saying no to drugs.
Can it hurt you? In the hands of the wrong therapist, yes. As I said in the last post, it can further destabilize initially until a protocol that works for that person is found. For a stable epileptic, tolerating meds, it may not be a good idea. For someone on the brink of harming themselves or others, it may not be a good idea, unless done in a controlled setting. For someone who has not tried meds, or wants off of them? For almost anyone with a neuropsychiatric disorder (and for those of you that haven’t read the DSM IV, that’s most of the entire human race), it’s worth a try.
I do think it’s worthy of comment here. There are people who say they are bothered by WiFi and on first glance, it sounds crazy, but one of things the internet and cell phones have done (also flourescent lights) is create an environment where we are constantly bombarded with electromagnetic frequencies which may entrain the brain to some extent towards poorer function and thus cause symptoms.
Now, oxygen reports and answers to some questions. I have heard from two more people reading the blog who experienced a flare of symptoms (herx) from the doses of normobaric oxygen I am using in my practice. I no longer think a herx is a good thing, but a potentially damaging cytokine storm, though I did see people push through it and improve with very high dose HBOT in my last practice. I now think that if that were to happen in my practice, I would back off, to maybe a half an hour every other day, see if that is helpful and go up from there. I would assume that those people would herx with hyperbaric also and it is possible that they could improve enough with lower dose oxygen that they would later tolerate the addition of pressure. All speculative for now. Anyone trying oxygen, please keep me informed. My practice is tiny and this is how I learn, how we are all learning for now.
I’ve gotten some questions which indicate that some don’t know the difference between a concentrator and a chamber. A concentrator puts oxygen directly into the room, through a tube, which is delivered to the patient in one of several ways- a cannula that goes in the nose, a simple mask, with holes in the side, or non-rebreather mask that has an oxygen reservoir that holds 100% oxygen and has one way valves to prevent inspiration of ambient air and to allow exhalation of exhalation gases. Oxygen can be brought to the home in tanks or in the form of a concentrator, that takes the oxygen out of the air. Tanks are quieter, but at the flows I’m using, need to be replaced frequently. Concentrators are noisy, but more portable and never run out. Concentrators can be portable or ultra-portable, but portables only give 2-4L/min (liters of flow per minute) and are used with a cannula (delivering 24-27% oxygen, instead of the 21% in air). A standard concentrator usually goes to 5 or 6L/min and can be used with a simple mask (delivering up to 35 or 40% oxygen). Some concentrators go to 10L/min and then can be used with a non-rebreather mask (delivering >60% oxygen depending upon fit). A non-rebreather mask should not be used without enough flow to inflate the bag.
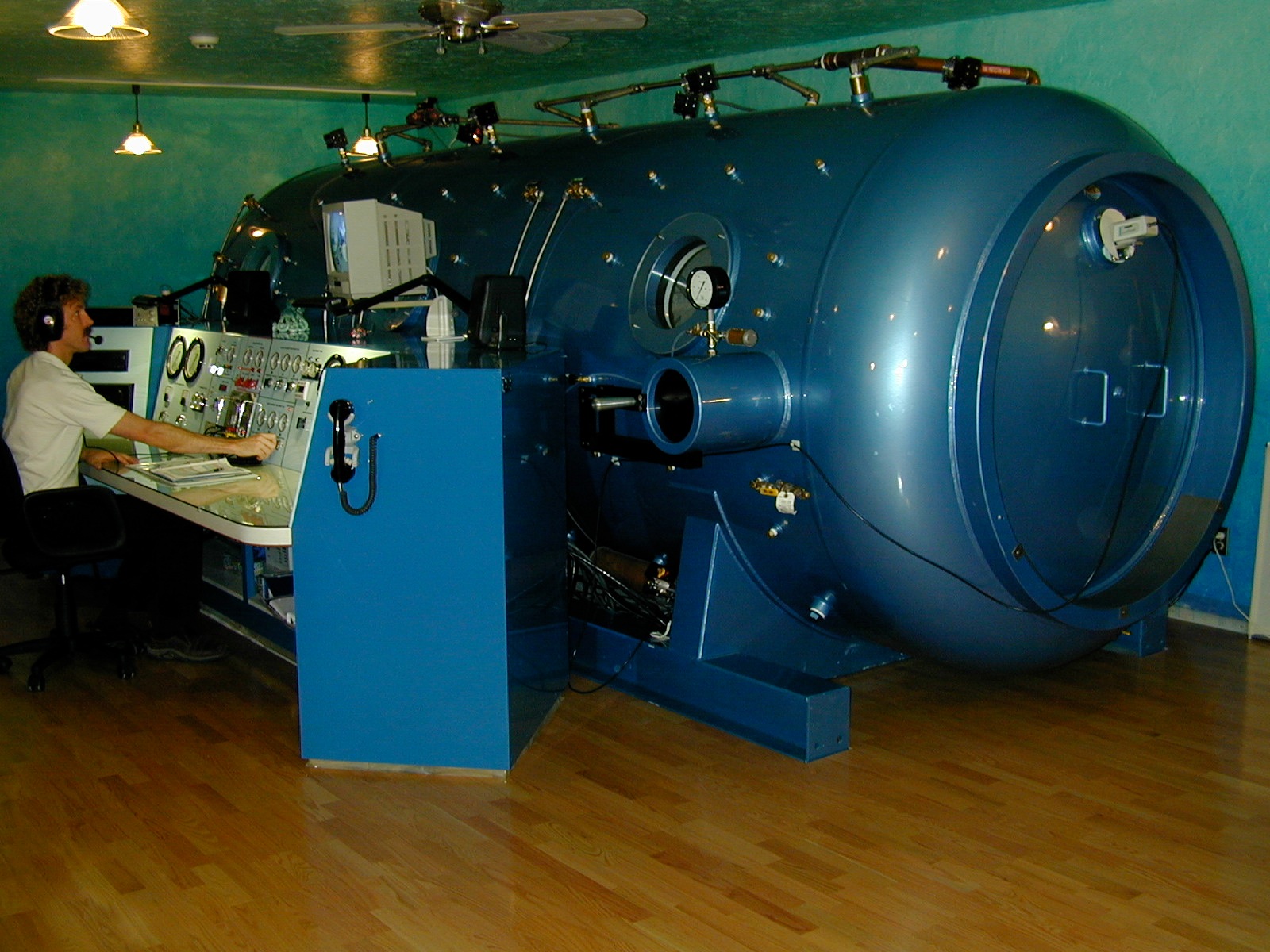
A chamber is a way to raise the ambient pressure of the patient above that in the room (normobaric pressure). Chambers can be monoplace, the patient goes into a 100% oxygen environment, or multiplace, multiple people go in together and oxygen is delivered by Scott mask or by hood, a bubble around the head with an airtight neckdam (latex or neoprene) to which oxygen is delivered with high enough flow to blow out the exhaled gases. Hard chambers go to pressures, or “depths”, of up to 3 ATA. Hyperbaric technology came from the need to treat divers with the bends. A huge amount of work has been done by the Navy and the commercial diving industry that has helped to elucidate the physiology of exposure to pressure and hyperoxia.
Sea level is defined as 1 ATA (measure of atmospheric pressure equivalent to 760mm Hg). 2 ATA is equivalent to the pressure at 33 FSW (feet of sea water), the way divers think of pressure. Depth and pressure can be measured in many ways; some common conversions are 1 atmosphere (atm or ATA) = 33 feet of seawater (fsw) = 10 meters of sea water (msw) = 14.7 pounds per square inch (psi) = 1.01 bar. The protocol generally used for treating brain injury is 1.3-1.5 ATA with 24-100% oxygen.
There is ongoing debate in the hyperbaric community as to whether the addition of pressure adds anything to a treatment that you could deliver without it. For example, there have been studies done showing that autistic kids respond to very mild hyperbaric treatments, 1.3 ATA and 24% O2. PaO2 = partial pressure of oxygen in arterial blood is between 75 mmHg and 100 mmHg at sea level (765 mmHg) on room air. A 1.3 ATA treatment with an FiO2 (fraction of inspired oxygen) of 24% will produce a paO2, or partial pressure of oxygen in the plasma of around 300mm Hg; you can get that with a mask and a concentrator, without a chamber (400mm Hg +). But my guess is, yes, it’s better with pressure. And our trail blazer K’s experience, a few blogs back, suggests that will turn out to be the case. A few references below re: possible independent pressure effects.
The breakthrough for hyperbaric treatment that allows it to be safe and simple enough for home use has actually happened since I left my last practice, in the form of the soft chamber. Gamow bags were developed to treat mountain climbers who develop altitude sickness. For this purpose, they are used without oxygen, simply adding pressure to increase the pO2 a little, and this works. It works by compressing the air so that the lung tissue is exposed to a greater number of O2 molecules in the same volume. In the early ’00’s I was worried about the possibility of an explosive decompression, which can be fatal, because the soft chambers sold are not rated for hundreds of duty cycles. But in practice, over quite a number of years now in home settings, it hasn’t happened. They do develop leaks on occasion, but slowly, and then they can be repaired. I see on the internet, there are quite a few newer companies selling cheap chambers, also some from China. I’d advise refraining from a bargain without a track record. To help with cost, I’ve heard of groups who live near each other sharing a chamber.
The chambers can be used with or without oxygen, though it says right on them that they are not supposed to be used with oxygen. Nevertheless, they provide a port to hook up your concentrator:). Oxygen should not be delivered directly into the open chamber, but through a mask, just as with a concentrator alone.
Oxygen saturation in blood, or O2 Sat, is measurable by pulse oximetry on the finger and expressed as a percentage. It tells you how much oxygen is getting through the lung into the blood. Since we don’t have trouble saturating hemoglobin, this number is often cited as the reason that we don’t need oxygen. However, it is possible to hyperoxygenate the plasma and we do have cellular hypoxia, meaning not enough oxygen is making it into the cell, or mitochondria (and/or it isn’t being metabolized properly). My guess is that there is an issue with oxygen getting across the mitochondrial membrane. Viral product from activated virus in mtDNA? Elevated anticardiolipin antibodies (and other autoimmune markers) are seen fairly commonly in the patient group. Cardiolipins are located on the inside of the mitochondrial membrane. Oxygen gets into the mitochondria by diffusion across a pressure gradient. Without enough oxygen, the cell can’t make ATP. If you raise the diffusion pressure, more goes in.
Relative contraindications to hyperbarics are seizure disorder, inability to clear ears for pressurization, though this should be able to be handled in almost all cases, without barotrauma, but takes patience on the part of the chamber operator, as well as good communication with the patient. Severe COPD with CO2 retention, is another relative contraindication, although in practice CO2 narcosis only happens in the setting of acute decompensation. Asthma is a concern, because wheezing can cause air trapping and a wheezing patient shouldn’t be decompressed as trapped gases will expand and cause barotrauma. Asthmatic patients should be pretreated. Hereditary spherocytosis because of red cell fragility. Pregnancy and cancer are considered relative contraindications because of the unknown, although there are hints that HBOT may in fact be helpful for cancer. Certain prior ear surgeries are a concern and should be discussed with an otolaryngologist. Also some eye problems should be carefully considered. Hyperbarics may accelerate the maturation of existing cataracts, though if this is true, it takes a lot; HBOT does not cause cataracts de novo, according to the literature. An exam by an ophthalmologist is a good idea prior to embarking on hyperbaric treatment. There have been cases of optic neuritis that worsened with hyperbaric treatments. Implanted devices should be checked prior to treatment with the manufacturer as to whether they are hyperbaric safe. The only absolute contraindictions to hyperbarics are the presence of an untreated pneumothorax (collapsed lung) and recent prior or concurrent treatment with doxyrubicin, cisplatinum, Sulfamylon or disulfiram (Antabuse).
Hyperbaric safety amounts to common sense. Don’t create sparks in the chamber as oxygen is an accelerant. It sounds like a simple thing, but there have been some terrible accidents, all due to human error. Only cotton should be worn in the chamber. Reading material is permitted, but not newsprint. Always make sure you have nothing in your pockets when entering a chamber.
There is a review on MedScape (here’s the link for those who can get in) from 2010 that lays out the party line, which is that only patients with certain very circumscribed indications should do it, but when you look into it further, it’s pretty clear that that is all about what insurance will and won’t pay for. Hospitals charge exorbitant per session prices and will only treat the indications that insurance covers. It is a global treatment. It affects every cell in the body and its potential uses are very broad. Risks low. The article also says that soft chambers are becoming popular (gasp) and that they can go to 1.5 or 1.7 ATA. DO NOT TRY THIS AT HOME. The soft chambers come with a pressure relief valve that prevents going above 1.3 ATA (aka 4 PSI). These can be disabled to allow higher pressures. The only accident I have heard about through the rumor mill involved someone who altered a chamber to go to 1.5 ATA. It doesn’t sound like much of a difference, but I’m sure there is an engineer out there reading who can put it in perspective for us. Amusingly, the Undersea and Hyperbaric Medicine Society defines a hyperbaric treatment as above 1.5 ATA.
A little interesting history of hyperbarics from the MedScape article:
Hyperbaric oxygen therapy (HBOT) is breathing 100% oxygen while under increased atmospheric pressure. HBOT is a treatment that can be traced back to the 1600s. The first well-known chamber was built and run by a British clergyman named Henshaw. He built a structure called the domicilium that was used to treat a multitude of diseases. The chamber was pressurized with air or unpressurized using bellows. The idea of treating patients under increased pressure was continued by the French surgeon Fontaine, who built a pressurized, mobile operating room in 1879. Dr. Orville Cunningham, a professor of anesthesia, ran what was known as the “Steel Ball Hospital.” The structure, erected in 1928, was 6 stories high and 64 feet in diameter. The hospital could reach 3 atmospheres of pressure. The hospital was closed in 1930 because of the lack of scientific evidence indicating that such treatment alleviated disease. It was deconstructed during World War II for scrap.
The military continued work with hyperbaric oxygen. The work of Paul Bert, who demonstrated the toxic effects of oxygen (producing grand mal seizures), as well as the work of J. Lorrain-Smith, who demonstrated pulmonary oxygen toxicity, were used with Navy divers. Exposure times to oxygen at different depths of water (and, hence, different levels of pressure) were quantified and tested based on time to convulsions.
This last work mentioned may be the source of the fear of oxygen. However, the Navy worked out the doses long ago. They have been using Nitrox, or oxygen enriched air, to prevent the complications of prolonged and repeated exposure to nitrogen bubbles produced during depressurization. Over time, hundreds of dives on air cause cognitive decline and joint disease. If you are diving with a mask in a multiplace or soft chamber, please make sure to wear your oxygen on the way up. There is huge experience from the diving industry that oxygen enriched air exposure, during exercise, is safe over many, many exposures. And that’s with pressure.
From this same MedScape article, which was written by detractors of alternative uses of HBOT:
Additionally, evidence is growing that HBOT alters the levels of proinflammatory mediators and may blunt the inflammatory cascade. More studies are needed to further elucidate this complex interaction.
And possibly pertinent to our patient group, although frank congestive heart failure is not typical of our illness…
As HBOT is known to decrease heart rate while maintaining stroke volume, it has the potential to decrease cardiac output. At the same time, through systemic vasoconstriction, HBOT increases afterload. This combined effect can exacerbate congestive heart failure in patients with severe disease; however, clinically significant worsening of congestive heart failure is rare.
I am weaning patients off fentanyl patches with oxygen concentrators and getting mail from all over the world from very sick people about how much it is helping them and thanking me. Oxygen is the best thing I’ve got to offer, not all by itself, but in synergy with other things. Of course not everyone benefits, but lots of people do and no one is harmed if used sensibly. If I could only do one thing for the sickest people, it would be to give them a concentrator to try daily for a while and during their worst moments. CFS doctors have bad mouthed oxygen for decades due to a logical fallacy, that because there is already oxidative stress, and oxygen produces temporary oxidative stress, during administration, that that is all it does, so therefore it is bad for us. As a result, patients have had to suffer more than necessary for a very long time. But no worries, soon those same doctors, who said oxygen was too dangerous to try, will be able to make lots of money giving everybody Ampligen and Rituxan.
Please read this wonderful paper:
Hyperbaric oxygen therapy promotes neurogenesis: where do we stand?
Numerous in vivo and in vitro studies confirm that HBOT induces neurogenesis however, underlying mechanisms remain unknown. Activation of several signaling pathways and transcription factors have been suggested to play an important role in HBOT induced neurogenesis, including Wnt, hypoxia-inducible factors (HIFs) and cAMP response element-binding (CREB)…
On HBOT and oxidative stress: HBOT enhances the production of reactive oxygen species (ROS) and causes oxidative stress in body tissues. Excessive accumulation of oxidative stress may contribute to neurodegenerative processes and cell death in the brain, as seen in diseases like Alzheimer’s disease (AD) and Parkinson’s disease (PD). Since HBOT-induced oxidative stress is directly proportional to both exposure pressure and duration, the benefits of HBOT, may outweigh the side effects due to the phenomenon of hormesis. Hormesis is a process that results in a functional improvement of cellular stress resistance, survival, and longevity in response to sub-lethal levels of stress. We suggest that this process might be beneficial in the treatment of oxidative stress associated neurodegenerative diseases like AD and PD.
Our data suggest that HBOT significantly ameliorates mitochondrial dysfunction in the motor cortex and spinal cord and greatly delays the onset of the disease in an animal model of motor neuron disease.
Dr. Rossignol believes that there is an independent pressure effect that induces mitochondrial biogenesis: This prior blog has links to some of Dr. Rossignol’s papers as well as slides from a lecture last year, and other oxygen references. The Next Step For Us. Here is one with an especially pertinent quote: The effects of hyperbaric oxygen therapy on oxidative stress, inflammation, and symptoms in children with autism: an open-label pilot study
This prospective open-label pilot study in children with autism indicates, as measured by changes in plasma GSSG, that HBOT ranging from 1.3 to 1.5 atm and 24% to 100% oxygen was not significantly associated with increased intracellular oxidative stress. The use of therapies to raise glutathione levels and lower oxidative stress before beginning HBOT in individuals with autism appears prudent. Among children with high initial CRP, hyperbaric therapy led to a large improvement in CRP levels; this suggests that inflammation in these children improved with treatment. Improvements in clinical outcomes as measured by several scales were observed at both 1.3 atm and 1.5 atm.
Here are some interesting random recent references:
Hyperbaric oxygen treatment for inflammatory bowel disease: a systematic review and analysis
Conclusions: HBOT lowered markers of inflammation and oxidative stress and ameliorated IBD (inflammatory bowel disease) in both human and animal studies. Most treated patients were refractory to standard medical treatments. Additional studies are warranted to investigate the effects of HBOT on biomarkers of oxidative stress and inflammation as well as clinical outcomes in individuals with IBD.
These data show that HBOT alleviates CCI-induced neuropathic pain and inhibits endoneuronal TNF-α production, but not IL-1β in CCI-induced neuropathic pain. Reduced TNF-α production may, at least in part, contribute to the beneficial effect of HBOT.
Thus, HBOT may present an option for the management of PSH (paroxysmal sympathetic activity) in addition to pharmacologic therapy. Potential mechanisms for these effects are discussed.
But whatever the mechanism, the proof is in the pudding. Relief is relief. Patients know it if they feel it. If it doesn’t make them feel better they can turn it off. The patients tell you what they need, if you listen. They tell you they have air hunger and are short of breath. Well, not at all surprisingly, oxygen can relieve it. The disease is characterized by diffuse vascular spasm. Even insurance companies will pay for oxygen for migraines. Unless you have CFS. Then you get nothing.
Today’s song: Black Muddy River
Erratum: De novo cataract development following a standard course of hyperbaric oxygen therapy. A recent paper reporting a case of de novo cataract formation after 48 HBOT sessions at 2.5 ATA for 90 minutes for chronic refractory osteomyelitis, an enormous dose compared to the doses discussed in this blog (high dose normobaric and mild hyperbaric treatments, all <1.5 ATA with 100% O2). There is a huge amount of wound care that has been done over many, many years now at the doses this patient was treated with and this case was considered reportable as a cautionary statement to suggest that it can occasionally happen at doses less than previously thought. As I said above, it is a good idea to get an eye exam prior to embarking on oxygen treatment and discuss any contraindications you might have. More importantly, if you try it and it works, you might want to involve your ophthalmologist in the decision to continue long term, especially if you have any pre-existing eye conditions.









“But no worries, soon those same doctors, who said oxygen was too dangerous to try, will be able to make lots of money giving everybody Ampligen and Rituxan.”
An insult does not go unnoticed. We all make choices as of whom we want to see.
Personally I don’t have a lifetime of magic medicine to try.
Real medication and real doctors for real disease.
Absolutely, Kati. Everybody gets to make their own choices. But it is the patient community that has been insulted, and not by me, but by pretty much the entire medical community. Neglected and abused for decades. These aggressive and dangerous intravenous medications are only palliative also, like the gentle things I am advocating. Rituxan, in particular, scares me for these patients. The immunological abnormalities are not yet understood well enough in the disease. It seems a potentially very destructive choice to me, even though there will be people who improve. The downside is too great. It kills people! Russian roulette.
I’m sorry if my comment upset you, because you are pursuing one of these paths, but it is my considered medical opinion.
If I die from this treatment- so be it. I made a very well informed choice for myself and I am comfortable with that. I know the risks, and I know the benefits. I have read the Fluge et al paper. I have professional experience with RItuximab. I have watched Fluge and Mella presentation from Invest in ME. I have talked with patients from Norway that have gone through the treatments. It is not for everyone. I know that for sure. Some other patients opted for Ampligen. And some other opt for very restricted diet, 2 or 20 handfuls of supplements (spending thousands of dollars) and alternative therapy. Their choice. Not mine.
As for costs for me, really, it’s probably comparable to travel costs, services and treatments that you offer to your patients which I note don’t include what you are personally taking to heal you from this damn disease. Too risky for your practice maybe? (but not for you)
Rituximab is covered for me, from patient assistance at Genentech. I am forever grateful to them and gladly give them all of my B-cells. They ain’t working.
And I am forever thankful for the Peterson, Kogelnik and the likes for offering these drugs to patients, and also organizing clinical trials- so we can actually tell for sure if it’s working or not. And for presenting and attending conferences like Invest in ME and IACFSME. Only through evidence based medicine can we move forward.
I am fed up with people wanting to cure us with fringe treatments. This in my opinion is not what we need. Real treatments. Real medicine.
I have never used the word “cure”. The treatments I am discussing reduce suffering and are quality of life enhancing, with or without Rituxan. If my ideas, knowledge and experience don’t interest you, that’s fine. No need to be insulting. Good luck to you.
And of course antiretrovirals are on the table for my patients, if you were implying they aren’t. I have one patient on Viread and two considering it. I consider all options with my patients. I just have a strong bias against treatments that can kill.
Well in fact I quoted you insulting physicians who have spent a lifetime taking care of us. While it is not necessary to make friends with these colleagues, at least giving them some respect would be good.
I seem to have touched a nerve here, and prefer not to engage any further. If you have decided to go this route, I leave you to your own decision and wish you the best of luck. I’m truly sorry that you can’t see the wisdom in the simple, gentle modalities I am discussing.
Dr. Jamie,
Please do not be discouraged by some unfortunate thoughtless posts. Maturity requires measured thoughts and comments. This is a lesson that many have yet to sufficiently learn. Your courageous, difficult, sincere, and meticulous efforts of your blog are literally saving lives and the quality of them. Thank you and keep up the good work!
I agree with Gk. Kati if you don’t like Dr Jamie’s approach you are free to go elsewhere. There are plenty of us who do like her common sense “first do no harm” approach. Calling these treatments “fringe” is an insult to all the patients who have been completely abandoned by mainstream medicine, whether it is the autistic community, the Lyme community or the ME community.
Oh, but I’ve gone elsewhere, danger mouse! :-) Couldn’t be happier
Katie if you’re so happy with your treatment and the treating doctors, why do you feel the need to come on here and say any of this, and make personal attacks on Dr Jamie who is sick herself and only trying to help people. It’s none of your business what treatment she is undergoing. What an inappropriate comment and nasty. You’re way out of line and don’t know boundaries. Attacking another ill person is wrong. Plenty of us are suffering, yet we don’t vent our spleen on others to feel better or feel one up. FYI my ME Spcecialist in Australia who has seen well over 5000 people with ME shares exactly the same thoughts as Dr Jamie on Rituximab, he said it’s great it’s been discovered but people have died from it. It’s not for me or people with ME BUT he said just wait, from this drug, better drugs will now follow. It’s discovery was a great thing. Personally I think you’re angry the Rituximab isn’t working for you and are displacing and projecting your anger on Dr Jamie. It’s understandable if you’re angry that your treament hasn’t worked so far, but please don’t direct your anger where it doesn’t belong. Own it, even if it’s hard to. I wish you the best.
Well Kati, let us know how well you were helped you out in about 25 years, and also the cost involved with all the treatments. Most of us have been in it awhile now. We already know. Bye bye.
Dr Jamie
I’m very interested in what you have written, I was just wondering do you test the oxygen status of the individual patient or are you treating blindly? This isn’t meant as inflammatory just a query. I’m presuming you check so forgive me if it sounds naive.
Thank you
Clare, your question is a good one. Transcutaneous oximetry is used in hyperbaric wound care. It is used to predict whether HBOT will help and to follow the course of treatment. Unlike pulse oximetry, which measures how much oxygen is bound to hemoglobin in the blood (expressed as a percent saturation), TCPO2 compares a distant normal site to the edges of the non-healing wound. However, the tissues we are interested in treating are deep. Brain tissue oximetry would require an implanted sensor, and most of my patients aren’t interested in that:). In addition to correcting local tissue hypoxia during an acute event, downstream of vascular spasm, we are intentionally creating a pulse of hyperoxia, which would be toxic if taken all the time. I’ve touched on some of the reasons why one might want to do this with the references above. There is also more information in prior blogs about oxygen:
http://www.x-rx.net/blog/2011/05/more-oxygen.html
http://www.x-rx.net/blog/2011/05/access-to-oxygen.html
And use the search feature in the header.
The safe use of hyperoxia, even under pressure, has been very well worked out by the diving industry, without the use of tissue oximetry. Scuba divers are routinely exposed to higher doses of oxygen, in Nitrox, than are used in clinical practice for brain injury. They are exposed repetitively for many years, and oxygen toxicity is more likely while exercising than at rest. The doses attainable with a concentrator are safe to experiment with, in my opinion. And unlike drugs, it goes away in minutes if you turn it off.
Again, we are not trying only to replace to a “normal” level of cellular oxygenation, which varies from tissue to tissue (and, in our case, I suspect moment to moment) anyway. Even if you could somehow do this, it would require wearing it all the time. Rather we are trying to hyperoxygenate for a prescribed period of time. I am trying to induce healing and reduce inflammation, by applying hyperbaric principles to a normobaric situation. Currently I am prescribing 1/2-1 hr a day for my patients, and more during the worst moments as well. I am trying to get the highest doses I can with the equipment at hand. If there is something to suggest it is too much, then back off. It seems the dose may be high enough for a very few people to get a die-off, or “herx”. Hyperoxia creates free radicals, and free radicals kill bugs. If this happened to one of my patients, I would back down, but not off. But, even with added pressure, treatment with 100% O2 by non rebreather mask at 1.3 ATA would take many, many hours of constant exposure to cause oxygen toxicity severe enough to induce a seizure in a non-epileptic person.
See for yourself , > Interviews with international researchers : http://electromagnetichealth.org/audio-archives-and-more/#levitt
Wireless technologies overwhelm all the signalling comprising biological processes .
WiFi is breaking BOTH strands of DNA— deformity will begin to show in the next generation.
WiFi permanently destroys mitochondria.
WiFi radiation accumulates in the body , like heavy metals.
Diabetes Type 3 is caused by wireless technology.
Healthy Russian teenagers have 90% increase of CNS and immune disorders since wireless began in 2000…
Ad Infinitum…
Connect the Dots
Jamie,
You are a violinist on the deck of the Titanic
http://www.youtube.com/watch?v=pj-1b1Yvep8
Another Samuel; could get confusing.
Samuel
Dr Jamie thank you for the wi fi info, that isn’t actually what I asked. Do you check the Transcutaneous Blood Gases before giving someone oxygen they may not actually need? With respect, yes or no would have been fine.
Just read the blog again, I think by what you say in this paragraph, the answer is no you do not check, it is up to the patient to tell you if it makes them feel better or worse.
“But whatever the mechanism, the proof is in the pudding. Relief is relief. Patients know it if they feel it. If it doesn’t make them feel better they can turn it off. The patients tell you what they need, if you listen.”
I am not criticising you, I have seen this treatment used but NEVER blindly, that is the point I am making.
That wasn’t Jamie answering about the wifi, that was a comment by someone else.
Answered your first question above, Clare. This is an important point. Let me know if it still isn’t clear.
Dear Jamie,
Many thanks for your great blog and sharing all of this info.
I’ve been looking into hiring an oxygen concentrator here in the UK (am mainly confined to bed). So far I have a quote back from one place, fairly expensive, and they say the concentrator offers up to 500L.min. This sounds very high from the figures you quoted.
I appreciate you are busy but may I ask what doses of normobaric oxygen you are using in your clinic?
Many thanks
@Annabel,
Something is wrong with the units. 5L/min? Maybe you misheard. I’d check back and ask for clarification.
I am using 5-10L/min for a half hour to an hour a day for home use, but most people manage it only 4 or 5 times a week, or even less and still are finding it helps. I am also starting to see declining use with improvement, even in people who responded very obviously at the beginning, and it seems to me that the sickest people are most likely to feel it tangibly. Also if used during an attack, migraine, palpitations, abdominal cramps, Raynaud’s, it is very useful. It makes people sleepy, so before bed is a good time to do it.
Hi Jamie,
Thanks for your reply. Yes, the woman from the company got back to me and apologised for writing 500L/min as opposed to 5L/min! Thought it sounded off….
This company only offers concentrators with flow of up to 5L/min. I was disappointed too at how expensive it is, £400.00 ($637) per month to hire and that doesn’t include tax which is around 20%. This is more than i can afford. It is the first company I came across so I will research some more. Would 5l/min be worth doing, as i know from your previous blogs your daughter used 10L/min and your aim is to get as high as possible if not able to use a chamber.
Many thanks
Ah, sorry, somehow missed your second paragraph, so you answered my question about whether 5L/min would be of any use.
I take it when you say you are seeing declining use after a time this is not because the oxygen treatment stops working, just that as the person is improving they don’t need to use it as much or frequently to get some benefit?
Really appreciate you taking the time to reply.
Yes, I meant that people tend to get a bit lazy when they start feeling a little better (like me:). But they still reach for it during the bad moments, and that’s when it helps the most obviously. When you are feeling ok, it becomes work to do it. Even though there’s not much to it, it’s noisy and you have to wear the mask.
However, at least for me, Ali and a few others, after overdoing, an hour of O2 prevents PEM. And then there’s the long term effect, slow, but stabilizing over time. Not everyone maybe, but enough to make it worth a try. Excellent risk/benefit ratio.
Thanks for the clarification.
I am going to give buying an oxygen concentrator some serious thought, as it sounds something that could benefit greatly…..
I’m trying at the mo to see if I could buy some cylinders and try that for a month before the financial outlay of buying a concentrator. Should i go ahead, I will post my experiences…
Many thanks for your help
That seems crazy expensive, Annabel. In the states, they run $150-$400/month. Tanks are much cheaper, but have to be changed out fairly often. Oxygen is regulated like a drug in the US, but laws vary country to country. I am unfamiliar with the laws in your country, but my understanding is that your hyperbaric trust, charity chambers, don’t require a prescription. Here a new concentrator requires a prescription. In some places, you can just go buy one. They are available used sometimes. I have a patient who bought a used 5L/min concentrator for $200.
Hi Jamie, yes, it is crazy expensive, but so far that is the price i keep getting quoted to rent. i could buy a concentrator at 5L/min for £700.00, so so far renting is not proving a financially feasible option.
Does a rental require a prescription in the UK? About $1200 is the price of a new 10L/min concentrator here. I have one patient who bought a refurbished one for $900.
Hi Jamie,
The rental companies I have spoken to haven’t mentioned requiring a prescription so far, but I might have missed it. The companies selling oxygen concentrators don’t seem to require a prescription. The prices do seem higher than the US. A 10L/min concentrator seems to cost around $2440/£1400. This is beyond my budget so should I go ahead and buy one it will have to be the 5L/min even though of course I would prefer the 10L/min. Thanks for all your help
Ive just spoken to a company that supplies the NHS and will rent out privately for a much more reasonable price, £50.00/month and a one off £150.00 supply fee. You do need a letter from your doctor though to sign off on you getting it. I really don’t know whether my GP would…, suppose only way to know is to ask…
Thanks for writing this article! What a timely blessing it has been for me.
I have a concentrator at home which I use with a cannula throughout the night. I qualified for Medicare because my oxygen consumption was 88% for 11 minutes using pulse oxometry. The concentrator is set at 2 L/min.
A sleep study ordered by my cardiologist revealed the problem. The symptoms which prompted him to have a sleep study done are morning headaches, abominable mornings where the word “fog” can’t begin to describe them, generalized weakness, and cognition problems. I will definately have him read your blog.
I just completed my 5th night and so far, so good. No headaches, MUCH better mornings. Of course, I need more time to make any real connection to the oxygen, and I hope I show improvement in other areas. Improved cognition would be great.
I didn’t read anything in your blog about using oxygen all night as I’ve been prescribed. How long do you have your patients use oxygen? What about my settings on the concentrator? Is this appropriate?
Thanks so much! You have and still are doing a wonderful thing for the CFS population.
Sleeping all night with low-flow oxygen to prevent desaturation during sleep is a different treatment, but I am hearing from people who are improving from this as well, with our without CPAP. This is a more obvious problem and physicians recognize home O2 as a good idea for this indication. What I am doing with pulsed high dosed oxygen is unfamiliar to most doctors. I would use pressure if I could, but pulsing oxygen with a high flow concentrator and a non rebreather mask is the highest pO2 I can get without a chamber.
Oops! Yes thank you Lilly! I should’ve checked that. I presumed someone answering a direct question to Jamie would have been Jamie! I will check twice next time. Thank you for pointing it out.
I found this article written in 2006 in the UK Action for M.E’s magazine, Interaction, about oxygen therapy and M.E. I thought it might be of some interest.
http://www.actionforme.org.uk/Resources/Action%20for%20ME/InterAction/InterAction%2050s/IA%2058%20A%20breath%20of%20fresh%20air.pdf
Interesting. My comments would take a whole ‘nother blog:). Thank you for posting.
Glad it was of some interest – although don’t want to generate more work for you in response ;-). Am sure there are comments in it that could be robustly challenged. It was interesting though that it did help some of those who gave it a good try….
For ME/CFS patients, the energy expended on getting the treatment is always an issue. My guess is that experiences with HBOT in the UK would be better with a home concentrator as well. The UK is blessed with almost free HBOT centers all over the country, thanks to the work of a very special doctor, Philip James. They will treat all neurological indications, including ME. For MS, they usually start with lots of treatments for a few weeks, then go to maintenance. For us, I’d probably try a concentrator first (like I did with K in the guest blog a few back). If clearly helpful, and once the patient’s body is used to some oxygen, HBOT might be even better. If so, maybe once per week? Start low, go slow is usually a good way to go for us.
Here is Dr. James’ website. I have been meaning to get in touch with him, and will do so now. I haven’t seen the site before, but I am sure, even without having read it yet, that this is the most accurate information on the subject available. Dr. Harch was a colleague and friend back then; I have been meaning to contact him again as well. Too much to do. Too little time…
http://www.hbotruth.com/physicians/james/james.html
Dr. Jamie,
Thanks so much for this excellent and informative blog post.
Does one need a doctor’s prescription to rent or buy an oxygen concentrator? What about for oxygen tanks? (I am in the United States.)
Keep up the good work!
In the US, oxygen is regulated as a drug and requires a prescription.
Can you please explain the benefits of a non-rebreather mask over a simple mask? A “simple mask” came with the oxygen concentrator I bought last summer.
Also, I do not understand how the term “non-rebreather” fits the mask in your picture. It would seem the exhalation being captured in the bag would cause one to re-breathe air they had exhaled.
Thank you so much for all your help, Jamie!
Hi Joy,
May i ask how you are finding the oxygen concentrator? Any benefits? No change?
Many thanks
Yes, I get an energy lift after using it that adds an hour or two of activity to my day. Now, I’m trying it right after exertion to see if it prevents PEM like Dr Jamie experienced, and I think I have had fewer crashes and less down time.
Thanks Joy for your reply, very appreciated
I’m sorry, I missed this and so didn’t answer sooner. A non rebreather mask has 95% oxygen in the reservoir, directly from the concentrator. There is a one way valve at the top of the bag, bottom of the inside of the mask, that prevents exhaled gases from entering the bag. There are also one way valves on the outside of the sides of the mask that allow exhalation but not inhalation of room air. These valves get lost a lot and need to be kept track of for the mask to work properly. The mask only functions properly if the flow rates are high enough to keep from rebreathing CO2, requiring a 10L/min concentrator. Please do not use a non rebreather mask with a low flow concentrator.
I thought this might be of interest..shows the HBOT treatments on rats helped with their neuropathic pain…
http://www.sciencedaily.com/releases/2012/04/120422162210.htm
Jamie, I hope it’s ok to ask a quick question. I have found a oxygen concentrator for a reasonable price that is 8L/min. I know 10L/min is optimal, but they are just so expensive here in the UK. Would 8L/min be better than 5L/min, even if not so good as 10L/min? If yes, I think I am going to buy it….big decision for me…
So I guess you need a prescription to breathe ? Sorry, just me with a lousy joke.