Believing I had written my least controversial blog ever, I am confronted yet again with how unconventional it is for a doctor to share their evolving thoughts publicly. If freely sharing information is revolutionary, what revolution are we talking about here? A departure from the science of evidence based medicine? Evidence based medicine is based on purposely flawed studies designed by drug companies to “prove” that their drugs should be prescribed. Drug companies make wild claims all the time, about drugs that have never had the test of time.
If Rituxan works for ME/CFS, that’s 4 million people in the US alone who need a drug that can cost upwards of $20,000 per round of treatment, including the high level of care needed to administer safely; it probably will need to be given twice a year, must be continued forever and carries a significant risk with each infusion. For fun, that would be $80 trillion dollars per year for us all to get treated. The drug is apparently much cheaper in the UK; it is going out of patent in 2015, so it will be cheaper in the US as well, but that also means there will be no funds to study it for us. The point is, it is not a sustainable model, this drug or another expensive palliative treatment. Nor would antiretrovirals have been had they worked very well. Too many people. And it’s not just this cohort, but several huge cohorts. Wouldn’t it make more sense at this point to figure out why so many people are getting sick with immunological diseases, rather than blindly killing everybody’s B cells? With monoclonal antibodies, produced from hybridomas, a fusion of mouse and human, technology that came from the very techniques that probably got us into this mess in the first place? It sounds like science fiction, but unfortunately it isn’t.
Look at this nightmare: Risk of autism among younger siblings of a child with autism much greater than previously reported. They say they are going to monitor future siblings now that they know their risk is about 18%, so they can offer early intervention to these incredibly high risk children. What intervention do they have in mind? CBT (ABA or Applied Behavior Analysis) to help them adapt to their brain injuries? How about considering the obvious and not vaccinating these particular children. That would be a rational approach, wouldn’t it? Let’s not challenge the immune systems of these particular children in this way, since they are at risk, and some of their siblings had problems with vaccinations? A little common sense? We have an obvious epidemic on our hands. We need to get everyone’s head out of the sand. How can society possibly take care of all these disabled children when they become adults?
It is the same for children of ME/CFS patients in my opinion. Though we don’t yet have the numbers, the informal survey from last year showed similarly alarming rates of CFS in offspring of CFS sufferers, as well as increased risk of autism, beyond even the alarming rates being acknowledged currently in the general population. These children should not be vaccinated in my opinion, or at the very least should be selectively vaccinated, with fewer total vaccines, fewer shots at one time and spread over a longer period of time. Common sense, except that we aren’t allowed to apply common sense when it comes to the vaccination program, because it is a sacred cow. We still intend to complete a formal family study. We are all working as hard as we can at our individual endeavors, but know how important this is. The incredible burden of disease that some families are dealing with needs to be brought into the light.
I encourage you to watch The Greater Good, a new documentary about childhood vaccines, the damage they are doing and the over the top blindness of our government’s approach to the problem. A special court to deal with the injuries. You can buy the DVD here. Please also visit and consider The Canary Party. Although it grew from concern about autism, it is about us too. The ME/CFS community desperately needs cross-pollination from the ASD community, politically and medically. They are related diseases and there is strength in numbers. Sharing between physicians could be rewarding for both groups. I still hope to do just that. I’ve launched a private forum to begin the dialog with the intention of sharing anything interesting or productive that comes out of it. All the participants are really busy, but want to share.
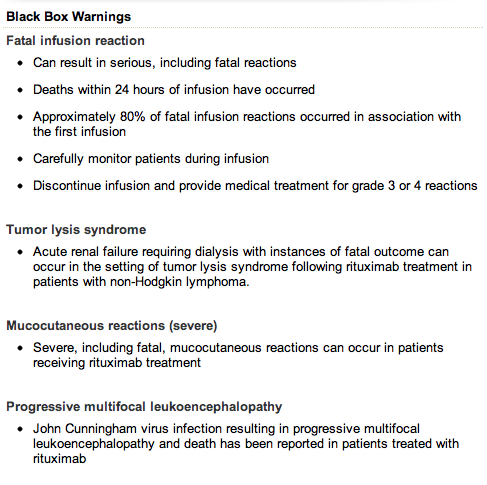
In the case of Rituxan, there is vast experience already, not for this indication, but a lot of experience for other indications. Enough that infectious disease doctors will tell you that it falls on them to treat the mess from JC virus reactivation, a fatal leukoencephalopathy, and cases of sepsis caused directly by the drug. That’s if the infusion doesn’t kill you, which granted, it usually doesn’t. I have a patient who is probably the perfect candidate for Rituxan, because she has the test results that would get it paid for, but her decision has been to wait, because the immunological abnormalities and variations in the patient group make it impossible at this time to select patients optimally. Meaning no way to know who will respond or precisely how to use the drug, until some patients have been the guinea pigs. There will be hits, as we saw from the Norwegian trial, assuming that we all have the same thing, which we probably don’t, but the biggest problem with Rituxan is that there will be deaths also.
Here are the black box warnings; all but tumor lysis syndrome apply to us:
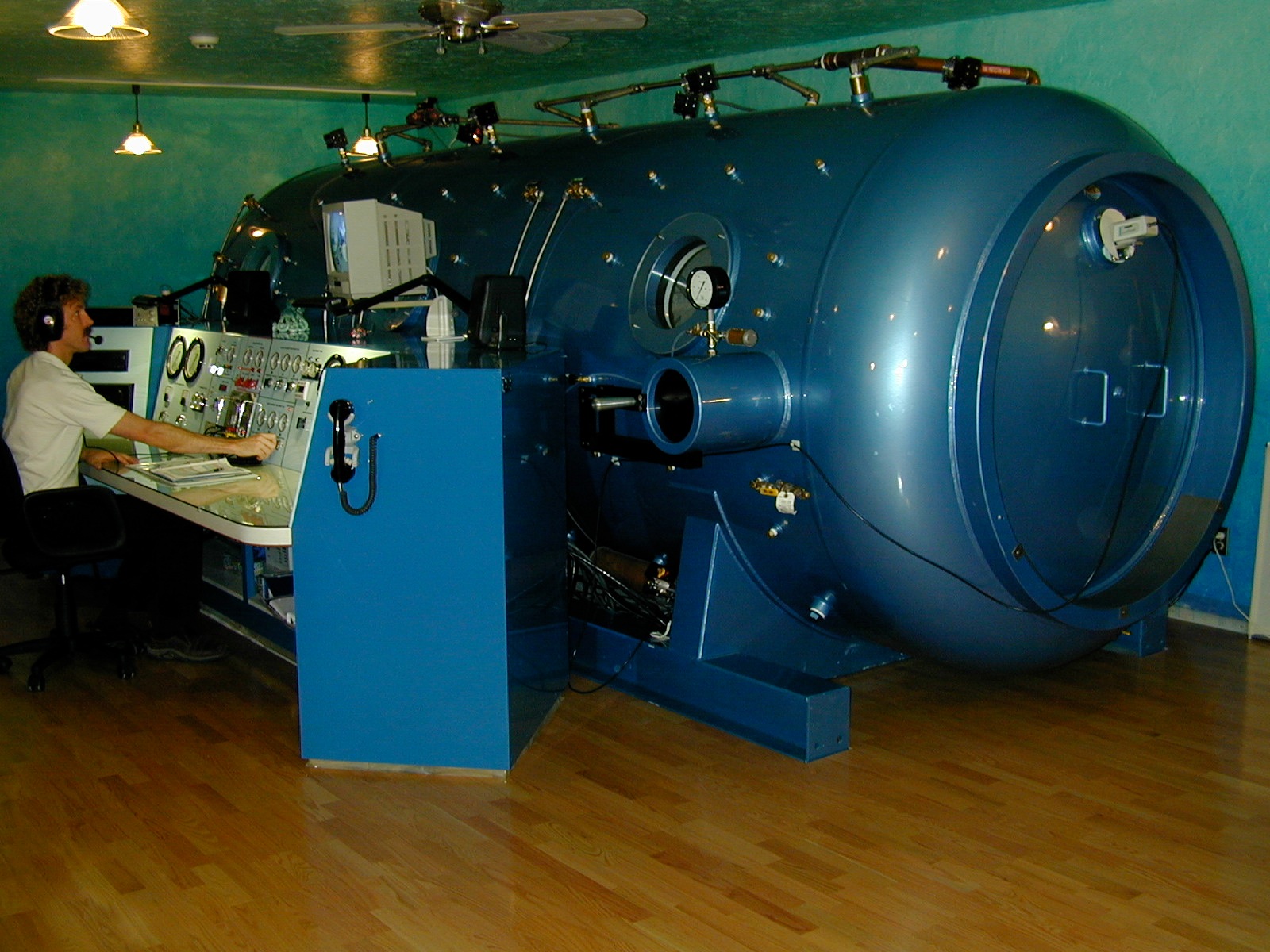
 Why do the gentle therapies bear the burden of proof? Because they don’t make money for the drug companies and the medical establishment? While doctors administer drugs that can kill with impunity, not even knowing precisely why they’re doing it, or what the long term consequences of it are, I’m expected to justify my “voodoo” with proof, and it doesn’t matter how many convincing references I come up with. Since it isn’t a drug, it couldn’t have value.
Why do the gentle therapies bear the burden of proof? Because they don’t make money for the drug companies and the medical establishment? While doctors administer drugs that can kill with impunity, not even knowing precisely why they’re doing it, or what the long term consequences of it are, I’m expected to justify my “voodoo” with proof, and it doesn’t matter how many convincing references I come up with. Since it isn’t a drug, it couldn’t have value.
I’m not trying to convince anyone to do anything. Everyone gets to make their own decisions. I am a medical libertarian. I’m not selling anything here. I started this blog before I was working. I have enough patients for what I can manage in my current state of health. I work in a very unusual, personal, hands on way and I am not right for everyone. In any case, I can only handle a very small number of active patients, especially if the intensive therapies that I’ve been writing about here are involved, so I am not writing to bring in business. I write for the same reason I wrote before I was in practice, trying to make a difference and save people from making the mistakes I made.
My writing is peppered with the anger that has been engendered by my patients’ histories, histories sent to me by email, and my family’s own history. Although I have returned to practice, I still identify most strongly with the patient group, not the doctor group. I hear from every well known CFS and Lyme doctors’ patients and it isn’t pretty. However, it is unfair to have your career contribution judged because of a few angry patients. Angry patients come with the territory and I acknowledge the inherent bias in who I hear from. I’m sure my being back in the same boat will make me more considerate of their constraints and decisions. In any case, not so much for the doctors, for some really do deserve the antipathy, but out of concern for the patients who respect them, I will refrain from gratuitous comments that divide us even further than we already are. I am getting a little tired of feeling like Don Quixote. I am not trying to convince anybody of anything and I could be wrong about anything. I am sharing my ideas, knowledge and experience, in case it helps someone. If it isn’t for you, that’s fine.
I am still hearing reports of benefit and reports of harm from various preparations of GcMAF’s and MAF yogurts. It does seem as if the opinions of the doctors managing these patients is now start low, go slow, always a good idea with ME/CFS patients, unless you are concerned about encouraging resistance of a microorganism. It isn’t clear how to tell when to stop or how to maintain an early effect. And I’m still disturbed by its being a completely unregulated blood product. Does anyone know if the newer MAF yogurts are derived from human blood?
I have always and still do tell patients that it is a bad idea to be in the first round of a drug trial. Let another million people take it first. I got called out by someone I respect for lumping Ampligen and Rituxan together and that is fair criticism. Ampligen has been around for a long time and it doesn’t kill people. Also I don’t know who is and isn’t making what money on either drug. My comment about doctors making money selling dangerous drugs was a general one, not aimed at anyone in particular, and certainly not limited to our disease. There are a very few CFS doctors who do manage to take Medicare or have been known to give away care and I acknowledge them for it. That is quite a feat with this patient group and the current system. At any rate, Ampligen costs a lot, and doesn’t seem like it works so well for many, or even most.
I would like to state for the record that I am not an angry person in my personal life. I have worked through much of my personal anger about how badly we were treated, mistreated actually, over the years. In fact, I am very happy now much of the time. I am laying down smile lines these days, not frown lines. Since you can’t see me, I want my readers to know that. My anger now is most often protective of my patients and friends. I would give anything if I could be proud of my colleagues more often, fully acknowledging that there is bias in the sample I am hearing from. Happy customers are less likely to write letters.
There is no cure and there isn’t going to be a cure, most likely. It is going to be about palliative care, at least for the foreseeable future. Hopefully it will also be about prevention, sooner rather than later, so we don’t have to feel so helpless watching while our friends’ children go down. Once you give up the idea of one drug to fix it, it becomes easier to see the wisdom of using multiple adjunctive therapies synergistically, all of which support the possibility of healing over the long haul, without harm.
My opinions about drugs aside, they are sometimes the best course of action and I still think that future treatment may include antiretrovirals, reverse transcriptase inhibitors in particular. The results of the uncontrolled patient experimentation that happened left a few of us on long term treatment that we think is helping; nobody was seriously harmed that I am aware of. The drugs in question are low risk. I have been reading and considering other reasons why RTI’s might be a good idea besides inhibiting exogenous retroviruses. It is a fascinating subject, taking us to the frontier of what is currently known about the human genome. Future blog fodder. The take home message from this blog is that I believe I can get to the same place with the therapies I am using, along with common sense primary care, without the risk, compared to any single treatment currently available. And I predict that my patients will do better over the long haul than allowing themselves to be used as human guinea pigs for the testing of dangerous drugs. Time will tell. However, it will always be only anecdote, not evidence based medicine. If my patients, friends and family are suffering less, it will have to do.
Today’s song: White Rabbit